During perimenopause and menopause, hormones like testosterone can dip, leading to a cascade of symptoms ranging from low energy and mood swings to hair loss. Many women may not realize that testosterone plays a crucial role in their health, alongside estrogen. But here’s the good news: There are foods that boost your testosterone levels naturally.
To learn more, we spoke with Greg Brannon, MD, FACOG, Medical Director at Optimal Bio, who explains the role of testosterone in women’s health and how incorporating specific foods into our diets can support hormonal balance.
What is testosterone?
When we hear the word “testosterone,” we often think of men. But this hormone is vital for women as well. “Testosterone is the most abundant active hormone in the human body,” explains Dr. Brannon. Produced by the ovaries and adrenal glands, “it becomes estradiol and is about 30 to 50 times higher than a woman’s estrogen. Testosterone affects every single cell and helps your body reach its optimal performance.”
This makes it essential for various bodily functions, which Dr. Brannon says include muscle development, bone density and strength. “Low testosterone levels can contribute to a higher risk of osteoporosis and fractures,” he adds.
While women produce much lower levels of testosterone than men, it still plays a significant role in sexual health, motivation and cognitive function, too.
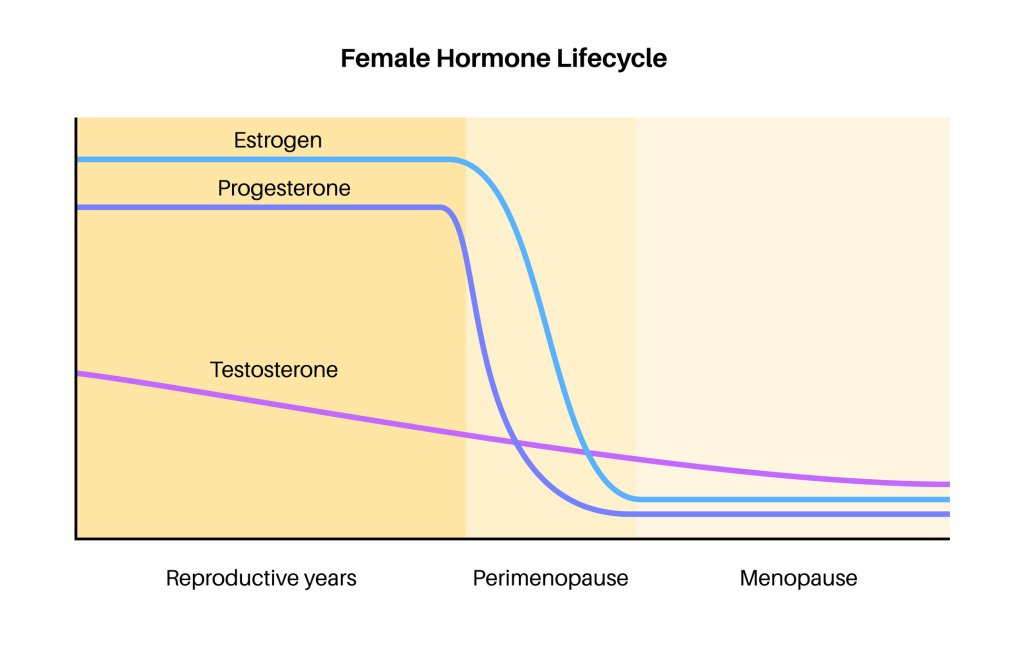
How menopause affects testosterone

Menopause is a phase of life that brings about profound hormonal changes. “It’s not just a lack of estrogen, but rather, a lack of all sex hormones (including testosterone and progesterone),” says Dr. Brannon. “These hormones are not just for reproductive purposes; every cell needs them. During menopause, women with low levels of testosterone may experience symptoms such as”
How diet impacts testosterone
“Our diet plays a significant role in determining which types of food support the production of testosterone in our body,” emphasizes Dr. Brannon. He notes that foods rich in zinc, vitamin D, omega-3 fatty acids and healthy fats are particularly crucial for testosterone synthesis.
According to Dr. Brannon, it’s not just about what you add to your diet but also about avoiding things that could harm hormone production, like highly processed foods and excess sugar. “A diet high in processed foods, refined carbohydrates and added sugars can also contribute to low testosterone production. Processed foods often lack essential nutrients and antioxidants that support overall hormone health.”
5 foods that boost testosterone naturally

Below are some top foods that can help increase testosterone production:
1. Fatty fish
Fish like salmon, mackerel and sardines are rich in omega-3 fatty acids. And fatty fish are fantastic for your overall hormone health. Omega-3s help reduce inflammation, which can indirectly support hormone balance, including testosterone.
2. Spinach
This dark, leafy green is a powerhouse of magnesium, a mineral that has been shown to improve testosterone levels. It also provides a range of other health benefits, including boosting energy and muscle function.
3. Oysters
Oysters aren’t just an aphrodisiac; they’re also packed with high levels of zinc, a mineral known to support testosterone production. Zinc helps regulate hormone levels, which is crucial as women go through menopause.
4. Avocados
Avocados are rich in healthy fats and contain both magnesium and vitamin D, making them a perfect addition to your diet for hormone health. “It’s important to consume high-quality natural fats like avocados,” says Dr. Brannon. “This helps reduce insulin resistance and appetite and keeps your hormones in check. Avoid seed oils and trans fat (which is unnatural and the body can’t eliminate).”
5. Grass-fed beef
“It’s higher in omega-3 fatty acids [than regular beef] and has vitamin E and vitamin A,” says Dr. Brannon. “Protein is important to add to your meal, as it provides essential amino acids in your body that help maintain muscle, skin and bone health. Furthermore, protein affects the release of hormones ghrelin and leptin, which control appetite.” Eggs and nuts are also a good source of protein.
Foods that boost testosterone: The bottom line

Remember, no single food or supplement will magically balance your hormones. Instead, think of these foods as part of a broader lifestyle approach that includes regular physical activity, stress management and adequate sleep. If you suspect your testosterone levels are low or if you’re experiencing significant symptoms, talk with your healthcare provider.
This content is not a substitute for professional medical advice or diagnosis. Always consult your physician before pursuing any treatment plan.



